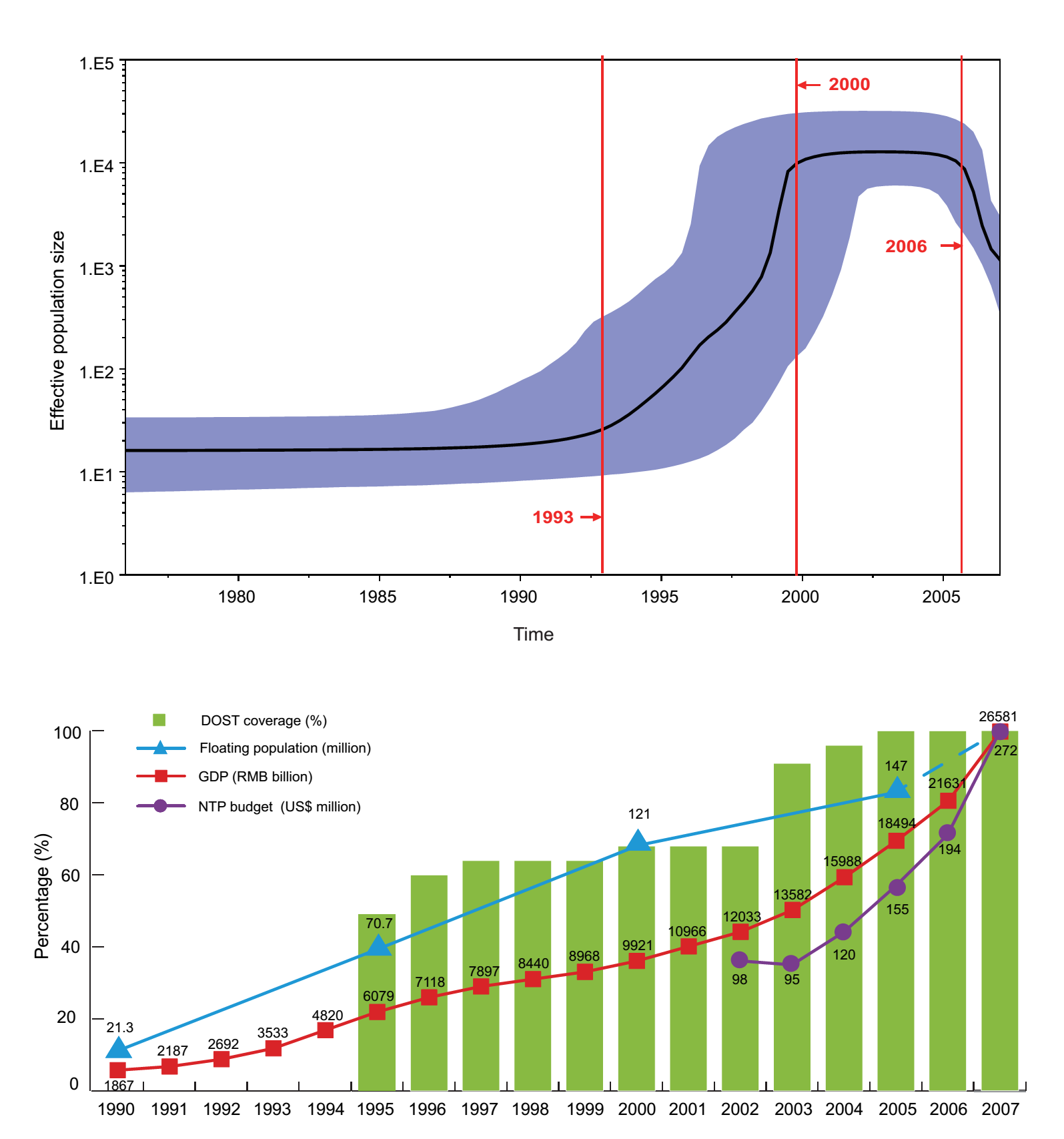
Beijing Institute of Genomics and other panoramic analysis of multidrug-resistant tuberculosis in China November 07, 2018 Source: Chinese Academy of Sciences Recently, the Chen Fei Research Group of the Beijing Institute of Genomics of the Chinese Academy of Sciences collaborated with the Beijing Chest Hospital and the National Tuberculosis Clinical Laboratory Xu Shaofa and Huang Hairong to collect 4,600 samples from the National Baseline Survey on Tuberculosis Resistance. Obtained 357 multi-drug resistance (MDR) tuberculosis strains, and carried out large-scale genome sequencing, combining the most comprehensive antibiotic susceptibility test (18 anti-tuberculosis drugs) and flow data to date, revealing China Epidemiology/drug resistance characteristics of MDR-TB, specific resistance genes and SNPs, and the history of MDR-TB strains in China. The collection of the study covers 70 districts and counties in 31 provinces, municipalities and autonomous regions, and is a comprehensive analytical study of multidrug-resistant tuberculosis in China. The results were published online in the journal International Infectious Diseases on the topic of Cross-sectional whole-genome sequencing and epidemiological study of multidrug-resistant Mycobacterium tuberculosis in China. According to the WHO Global Tuberculosis Report, tuberculosis has surpassed AIDS for the fourth consecutive year since 2014 and has become the world's number one infectious disease killer and one of the top ten most deadly diseases in the world. There are more than 10 million new cases of tuberculosis each year, and the death toll exceeds 1 million. At present, drug-resistant tuberculosis is still one of the most important causes of tuberculosis, and its mortality rate is extremely high. The cure rate is only 54%, posing a huge threat to global public health. The statistical results of this large-scale study of data on the flow of blood transfusion showed that the proportion of patients with multidrug-resistant tuberculosis was higher than that of the initial treatment, with obvious gender, population and regional characteristics. By calculating the resistance rates of 18 anti-tuberculosis drugs in multidrug-resistant strains, the researchers found that the resistance rate of pyrazinamide in the first-line anti-tuberculosis drugs was the lowest, and the beta-quinoline (0.8%) in the second-line anti-tuberculosis drugs. Dramani (1.4%) and linezolid (2.8%) have low resistance rates, and these three drugs are currently the preferred drugs recommended by WHO for the treatment of multidrug-resistant tuberculosis. The analysis of the prevalence of drug resistance in seven administrative regions of China shows that the drug resistance of multidrug-resistant tuberculosis in China is very serious. More than 50% of multidrug-resistant strains in China are resistant to more than 5 anti-tuberculosis drugs. Through Fisher's exact test analysis of the drug resistance patterns of multidrug-resistant strains in seven administrative districts, five first-line drugs have high-frequency co-resistance patterns, and other drugs include two kinds of fluoroquinolones, ofloxacin and moxifloxacin. In addition, they all exhibit low-frequency co-resistance patterns. Researchers combined drug-resistant phenotypes and genotype data to reveal the genetic basis of multidrug-resistant tuberculosis-resistant phenotypes using three statistics and a machine learning approach. 42 drug-resistant SNPs and 44 drug-resistance related genes were screened, and 31 drug-resistance related genes were first discovered in this study, which provided new targets for the diagnosis and treatment of drug-resistant tuberculosis. In addition, the results of Bayesian skyline analysis show that the change of population size of multidrug-resistant tuberculosis in China is closely related to China's economic and social environment and the construction of national tuberculosis prevention and control system. From 2000 to 2006, the population growth of multidrug-resistant tuberculosis in China was effectively controlled, and it showed a significant downward trend after 2006. This was mainly due to the increase in policies and funds of the government since 2000. Support for the prevention and treatment of tuberculosis. This study provides a solid data and theoretical basis for the accurate diagnosis and treatment of drug-resistant tuberculosis in China, and provides useful reference and reference for the prevention and control of global drug-resistant tuberculosis. The research was funded by the Ministry of Science and Technology's major special project on infectious disease prevention and control, and the key deployment projects of the Chinese Academy of Sciences. Factors Affecting the Size of Multidrug-Resistant Tuberculosis Population in China Peptide Powder,Collagen Powder,High Purity Ipamorelin,Bodybuilding Gdf-8 Myostatin Powder Shaanxi YXchuang Biotechnology Co., Ltd , https://www.peptide-nootropics.com